Abstract
1. Introduction
The introduction of direct oral anticoagulants (DOACs) has led to their widespread use for stroke prevention in patients with non-valvular atrial fibrillation (AF) and as first-line treatment in acute venous thromboembolism (VTE), and also as secondary thromboprophylaxis in patients with a history of VTE. In addition, many patients previously taking vitamin K antagonists (VKAs) have switched to a DOAC for reasons including erratic international normalised ratio (INR) control, medication interactions, convenience, possible lower major bleeding risk and possible improved stroke prevention rates. Although DOACs are well tolerated, little is known about the numbers of patients switching from a DOAC to (or back to) a VKA or the reasons for doing so.
2. Methods
This study was an analysis of prospectively-collected data from a four-year period surveying a computer-based VKA (warfarin) dose adjustment clinic in a large city centre hospital. The primary objective was to identify the reasons for patients switching from a DOAC to warfarin. Secondary objectives included assessing indication for anticoagulant therapy and choice of DOAC. The time in therapeutic range (TTR) once switched back to VKA and clinical events following commencement of warfarin were also determined.
3. Results
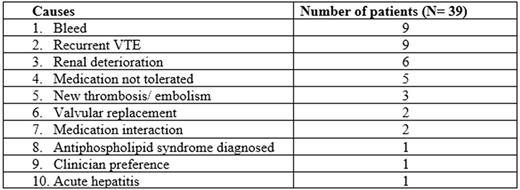
In our VKA clinic with 1791 patients annually under review, 39 patients were identified as having switched from a DOAC to warfarin. The mean age of the patients was 68.5 years +/- 13.8 and the majority (N=24) were female. AF was the most common condition necessitating anticoagulation (N=24); VTE accounted for 12 cases; arterial thromboembolism (N=2) and cardiac thrombus (N=1) were less common causes and one patient had been started on a DOAC in the setting of valvular replacement. Of the patients who were switched to warfarin, seven (17.9%) had originally been anticoagulated with a VKA prior commencing on a DOAC. In terms of anticoagulant choice, the majority of patients (N = 27) were taking rivaroxaban with 6 patients each on dabigatran and apixaban. The causes for switching in this cohort are outlined in table 1. Interesting cases of note include one patient who had a splenic infarction while taking rivaroxaban for atrial fibrillation and one patient who developed a new thumb arterial embolus while taking rivaroxaban for a PE.
Following warfarin commencement, there was a total of eight clinical events reported (21.1% of patients). There were seven bleeding events recorded with two serious events necessitating hospital admission and five minor events; in five of these (71.4%), the original reason for switching back to warfarin had been a bleed while on a DOAC. One further patient had a high INR necessitating administration of vitamin K. The mean TTR of this cohort was 61.4% +/- 22.3. 33 patients (84.6%) of patients still attend the warfarin clinic, with cessation of anticoagulant therapy having occurred in three patients (7.7%) and death occurring in one patient (2.6%); two patients (5.1%) have been recommenced on a DOAC.
4. Discussion
DOACs have several advantages over warfarin for many patients; they do not require monitoring and the dose remains stable. Index trials have demonstrated at least non-inferiority to warfarin in stroke prevention in non-valvular AF and treatment of VTE, with at least no significant difference in bleeding outcomes. However, warfarin can be an attractive option in complicated cases as it can be rapidly reversed, and there continues to be greater levels of clinician experience with its use. In the present study, we report data regarding the switch back to warfarin in a DOAC cohort, an area into which little research has been conducted. There were only 39 patients reported over a four-year period; this represents only a small minority of the full cohort. As expected, the majority of patients required a switch because of re-thrombosis or a bleeding event. Patients also required an appropriate switch in situations outside of the licence of the DOACs i.e. renal deterioration or valvular AF. The authors are not aware of any data regarding arterial embolisation in rivaroxaban users, and acute hepatitis has been rarely described in rivaroxaban use. These data confirm that switching from a DOAC to warfarin is seldom deemed necessary by clinicians. However, familiarity and experience may guide therapy in complicated cases, and vigilance is required to ensure adherence to the licence when prescribing a DOAC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal